For the early onset of pregnancy, it is important to know and be able to determine the days when ovulation occurs, since the conception of a child occurs on such days. This article will describe how to determine the onset of ovulation.
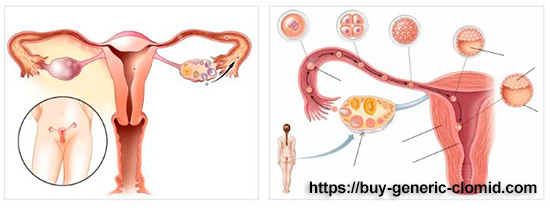
Ovulation is the process of leaving a Mature and fertilized egg from the ovary. The menstrual cycle of a woman is so arranged that in its first phase there is maturation of follicles and eggs in them (normally it is one or two eggs), which at the time of ovulation come out and are ready for fertilization. With the help of the fallopian tube, they enter the uterine cavity, where they merge with the spermatozoa. If this does not happen, then the egg dies, and the second phase of the cycle will help to remove it and prepare the uterine cavity and endometrium for the next attempt.
For the early onset of pregnancy, it is important to know and be able to determine the days when ovulation occurs, since the conception of a child occurs on such days.

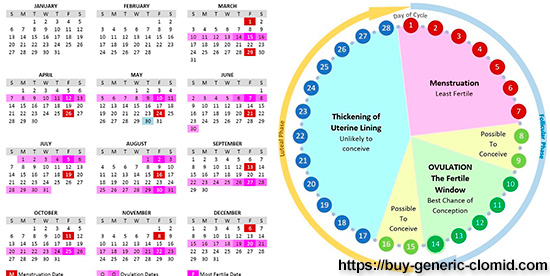
The egg Matures during the menstrual cycle, which is necessary for the preparation of the uterus and the maturation of the egg, the result of which is ovulation. To determine ovulation using the calendar method, you need to know your menstrual cycle for the last few months. Knowing the cycle, you can calculate its length, i.e. the interval from the beginning of one month to the beginning of the next.
14 days are subtracted from the total duration of the cycle. So, if the cycle is 28 days, then taking away 14 days, we get 14 days of the cycle, in which the egg can exit the ovary. For conception within a week before ovulation and after it, the couple is recommended to have an active sexual life, preferably with breaks of 1-2 days, in order to have time to Mature the spermatozoa. As already calculated above, the release of a Mature egg occurs somewhere in the middle of the menstrual cycle.
Ovulation is the only day when you can get pregnant, without it, the onset of pregnancy is impossible. This is a very fast phase, which ends immediately after the release of a Mature egg from the follicle.
The ovulation cycle is usually divided into several periods: preovulation, ovulation itself, and postovulation. Nature created man so that he could have at least a day to conceive before or after ovulation. Why so? all because if the onset of pregnancy was possible only during ovulation, then there would be much more problems with infertility, and thanks to some life of the egg after ovulation, this period increases, which makes it possible for couples to fertilize and reproduce. In all women who are of reproductive age, there is a fertile period, which implies the time of pregnancy. This time falls on the ovulation itself and 3 days before and 2 days after it. This period is associated with the life of a sperm that lives in a woman’s body for up to five days.
Ovulation in women of childbearing age occurs periodically (every 21-35 days). The frequency of ovulation is regulated by neurohumoral mechanisms, mainly gonadotropins of the anterior pituitary and ovarian follicular hormone. Ovulation is facilitated by the accumulation of follicular fluid and thinning of ovarian tissue located above the protruding pole of the follicle. The constant ovulation rhythm for each woman undergoes changes within 3 months after abortion, within a year after delivery, and after 40 years, when the body is preparing for the pre-menopausal period. Ovulation stops with the onset of pregnancy and after the extinction of menstrual function. Setting the ovulation period is important when choosing the most effective time for fertilization, artificial insemination, and in vitro fertilization.
Signs of ovulation
To determine the day of ovulation, knowledge of its signs will help, for which it is necessary to treat your body with great attention. Of course, ovulation can not always be suspected, because its manifestations are very subjective and sometimes go unnoticed by a woman. But the changes in the hormonal background that occur every month allow you to “calculate” and remember the sensations during ovulation and compare them with the new ones.

Subjective signs
The subjective signs of ovulation are those that a woman feels and only she can tell about. Another name for subjective signs is sensations:
Abdominal pains
One of the first signs of ovulation is considered to be pain in the lower abdomen. On the eve of the rupture of the follicle, a woman may feel, but not necessarily, a slight tingling in the lower abdomen, often on the right or left. This indicates a maximally enlarged and strained dominant follicle that is about to burst. After its rupture, a small wound of several millimeters remains on the ovary shell, which also bothers the woman. This is manifested by minor aching or pulling pains or discomfort in the lower abdomen. Such sensations disappear after a couple of days, but if the pain has not passed or is so acute that it violates the usual lifestyle, you should consult a doctor (ovarian apoplexy is possible).
Mammary glands
There may be soreness or hypersensitivity in the mammary glands, which is associated with hormonal restructuring. FSH production stops and LH synthesis begins, which is reflected in the breast. It is swollen and rough and becomes very sensitive to touch.
Libido
Another characteristic subjective sign of approaching and coming ovulation is an increase in libido (sexual desire), which is also due to hormonal changes. It is so predetermined by nature that it ensures the continuation of the genus – once the egg is ready for fertilization, it means that you need to strengthen your sexual desire to increase the probability of sexual contact and subsequent pregnancy.
Aggravation of sensations
On the eve and during ovulation, a woman notes an aggravation of all sensations (increased sensitivity to odors, changes in color perception and taste), which is also explained by hormonal changes. Emotional lability and sudden mood changes (from irritability to fun, from tears to laughter) are not excluded.
Objective sign
Cervix uteri
During the gynecological examination in the ovulatory phase, the doctor may note that the cervix has softened somewhat, the cervical canal has opened slightly, and the neck itself has lifted up.
Oedemata
Swelling of the limbs, most often the legs, indicates a change in the production of FSH to the production of LH and is visible not only to the woman herself, but also to her relatives and the doctor.
Excreta
When ovulation changes its character and vaginal discharge. If in the first phase of the cycle a woman does not notice spots on her underwear, which is associated with a thick plug that clogs the cervical canal and prevents infectious agents from entering the uterine cavity, then in the ovulatory stage, the discharge changes. The mucus in the cervical canal is liquefied and becomes viscous and viscous, which is necessary to facilitate the penetration of spermatozoa into the uterine cavity. In appearance, the neck mucus resembles egg white, stretches up to 7-10 cm and leaves noticeable spots on the underwear.
Basal temperature
This symptom can only be detected by a woman who regularly keeps a schedule of basal temperature. On the eve of ovulation, there is a slight (0.1-0.2 degrees) decrease in temperature, and during the rupture of the follicle and after the temperature rises and remains above 37 degrees.
What does ovulation feel like?
What does a woman feel during ovulation? Every woman who carefully monitors her female health can clearly tell the time when ovulation is approaching and when it occurs. Among the signs that indicate the approach of ovulation, highlight the nature of the discharge – they become thick, abundant and transparent. Additional symptoms include:
- discomfort in the lower abdomen
- breast swelling, mild soreness
- an increase in basal temperature, if its schedule is determined by a woman
- sexual desire reaches its maximum
Fortunately, the severity of clinical symptoms of ovulation in most women is so minimal that they do not attach importance to them. Others also note during this period of pain in the lower abdomen on one side, which indicates which ovary ovulated, heaviness in the lower back, which independently disappear after a short period of time. And only a small percentage of women note a pronounced pain symptom that forces them to seek medical help.
We have discussed how to determine ovulation by feeling a little, but it is important to remember that not all women observe such symptoms and this does not allow us to talk about the lack of ovulation in them, because their pain threshold is so high that they level these feelings. You can reliably confirm the presence of ovulation only by measuring basal temperature, conducting ovulation tests, or using ultrasound, which determines the observation of the growth of follicles and the exit from the dominant egg, as well as a sharp change in vaginal secretions allows you to judge the onset or approach of ovulation.
The duration of ovulation
Every woman who plans to give birth to a child should know how many days ovulation lasts in women and by what methods it can be calculated. Ovulation itself involves the release of an egg, ready for fertilization, from the dominant follicle, which breaks under the influence of hormones and in its place a yellow body is formed.
How many days is ovulation in women and how to determine it? All women are interested in this issue at the stage of pregnancy planning, especially if the process of fertilization does not occur for a long time. Everyone knows that pregnancy requires ovulation, and the time of its onset falls in the middle of the menstrual cycle. But, unfortunately, not every woman has a regular menstrual cycle, which allows you to determine its time of onset. Almost every woman who is of reproductive age can become pregnant in the middle of the menstrual cycle for several days. To calculate the time of ovulation you need to use several methods:
- the standard method is that after two weeks from the first day of menstruation, the probability of ovulation increases, but this is not for everyone. This method works if the menstrual cycle lasts 28 days. If the cycle is longer, then the onset of ovulation occurs later.
- measurement of basal temperature from the first day of the cycle in compliance with all the requirements, because during ovulation in the body there is a hormonal adjustment, which is characterized by an increase in temperature on the graph and indirectly indicates ovulation. This method can be judged after several months of observation. The onset of the upcoming ovulation can be judged by a sharp decrease in temperature due to hormonal imbalance and its subsequent increase above 37 degrees
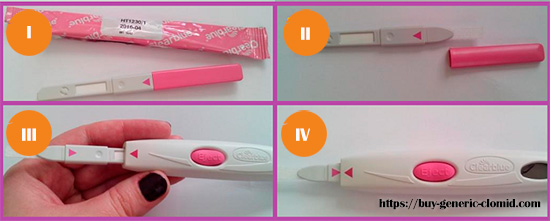
- ovulatory tests make it possible to study ovulation for several days, which is very important when planning a pregnancy
Ovulation lasts on average from 16 to 32 hours, but this is the time of the fertile window, that is, the time when it is possible to fertilize the egg and the onset of pregnancy. The release of a Mature egg itself lasts from a few minutes to a dozen minutes, which was noticed during IVF.
To determine how long ovulation lasts in women, you can use its characteristic signs: increased libido, swelling and swelling of the mammary glands, discomfort in the lower abdomen and lower back, more on the one hand, abundant mucous discharge, sometimes with streaks of blood.
How long ovulation takes depends on the lifetime of the germ cells. A Mature egg that has emerged from the follicle can be fertilized within one or two days, which is always individual. Therefore, if a woman has symptoms of ovulation on one day, then the next two days may also be the onset of ovulation, as well as sexual intercourse three days before it often leads to the onset of pregnancy, because the sperm lives about three days.
How many days is ovulation — each woman can determine by clinical symptoms, and if the vaginal discharge disappears or becomes too thick, pain and swelling of the mammary glands disappear, then we can say that it has passed, and the probability of pregnancy is not.
The period of ovulation in women can fluctuate with inflammatory processes in the reproductive system, with eating disorders, significant physical and mental loads, with severe stress and nervous shocks, with a sharp change in climatic conditions of residence, as well as with active sexual life.
Do not forget that the body can have both early ovulation and late ovulation. Early ovulation is characterized by its early onset and is associated with frequent sexual acts, significant physical activity, strict diets, as well as the presence of diseases that can affect the hormonal background of a woman. Sometimes ovulation comes late, which can also be determined using the tests and techniques that we discussed a little earlier. Due to the presence of ovulation and the regularity of the menstrual cycle, it is possible to indirectly judge a woman’s reproductive age, her probability of pregnancy and gestation. Many women, knowing when they are ovulating, plan a pregnancy or carefully protect themselves from it. The absence of ovulation for 2 or 3 cycles indicates a violation of reproductive health and requires medical attention to correct the hormonal background.