Clomid (clomiphene citrate) is a highly effective antiestrogen officially classified as a selective estrogen receptor modulator (SERM). Review of clomiphene citrate: In many ways, it is very similar to the other popular SERM in Nolvadex (Tamoxifen Citrate). Clomid first gained worldwide attention in the early 1970s as a powerful fertility enhancer and is still used for this purpose. It is also one of the most commonly used SERMs by anabolic steroid users. No, this is not an anabolic steroid, but it can be used to combat the estrogenic side effects sometimes caused by anabolic steroids. It can also be used as a post cycle therapy (PCT) medication to stimulate suppressed testosterone production due to anabolic steroid use. The use of PCT-based Clomid is the most common target and most beneficial point of use for anabolic steroid users.
Functions and features of Clomid:
Clomiphene citrate is a SERM that is specifically used as a fertility aid due to its ability to increase the release of gonadotropins. Clomid has the ability to counteract negative estrogen feedback on the hypothalamic-pituitary-ovarian axis. This will significantly increase the release of luteinizing hormone (LH) and follicle stimulating hormone (FSH). By increasing the release of gonadotropin, this can lead to the release of an egg, thereby increasing the chance of conception.
Clomid also has strong antiestrogenic properties that can be used therapeutically, but its antiestrogenic properties are most commonly associated with anabolic steroid use. Testosterone and many testosterone-derived steroids have the ability to convert to estrogen through the interaction of testosterone with the aromatase enzyme. An increase in estrogen levels can lead to gynecomastia and water retention. Water retention in the body can also contribute to high blood pressure. By adding Clomid while using anabolic steroids, the SERM will bind to estrogen receptors, thus preventing the estrogen hormone from binding. This can be very helpful in the fight against gynecomastia because when Clomid binds to the receptor, it prevents estrogen from stimulating the breast tissue. It can also have a positive effect on water retention.
Clomid also has functional characteristics that are beneficial for anabolic steroid users after consuming anabolic steroids. In particular, we are referring to post cycle therapy (PCT). In men, Clomid also has the ability to stimulate the pituitary gland to produce more LH and FSH, which in turn stimulates increased natural testosterone production. This is extremely beneficial for those taking post cycle anabolic steroids as natural testosterone levels will be very low due to the suppression caused by anabolic steroid use.
Effects of Clomid. Review of clomiphene citrate
In therapeutic settings, as a fertility aid, Clomid has a simple effect. A woman has difficulty getting pregnant, Clomid increases the likelihood of conception and pregnancy. This doesn’t always work and we’ll go through the process in the administration section, but it will greatly increase the chances of conception and is quite successful.
As an antiestrogen when using steroids during a cycle, Clomid is quite effective in preventing gynecomastia. It does not lower estrogen levels or inhibit the aromatization process, but in many cases receptor binding is sufficient protection for many men. In fact, even though stronger protective agents exist, many men would be surprised how well a SERM like Clomid can work if they gave it a chance. More importantly, using Clomid for this purpose can also positively affect cholesterol levels. Although Clomid is an antiestrogen, it actually acts like estrogen in the liver, which in turn promotes healthier cholesterol levels. This can be very beneficial for an anabolic steroid user as anabolic steroid use is known to increase unhealthy cholesterol levels.
For many men, especially heavy anabolic steroid users, Clomid is not enough to protect against estrogens. In this case, an aromatase inhibitor (AI) such as Arimidex (Anastrozole) or Femara (Letrozole) will be required. AIs actively suppress the aromatase process, and serum estrogen levels decrease. By far, they are the most effective in combating gynecomastia and more effective in combating water retention. In fact, SERMs like Clomid often do very little to combat water retention.
However, in many cases, many athletes would be better able to control their water retention if they had more control over their diet. In the off-season, to gain mass, this requires an increase in the number of calories. However, many go too far, especially when it comes to carb intake, and this forces you to hold back with or without anabolic steroids. Add flavoring steroids to the equation and water retention is even greater. Also, AI, while effective, will have a negative effect on cholesterol, which leads us to only one reasonable conclusion. Control your diet and if you can control gyno with a SERM like Clomid, this should be your first choice.
We are then left with the effects of Clomid as they relate to PCT. When we take anabolic steroids, it suppresses the natural production of testosterone. The rate of suppression will depend on the steroids used and to some extent on the total dosage, but will usually be significant. For this reason, most men always include exogenous testosterone in their steroid cycles. In fact, it is not uncommon for this to be the only steroid used. This will protect the person from low testosterone levels during the cycle. Unfortunately, once steroid use stops, natural testosterone levels will be very low. Natural testosterone production will start on its own again, but it will take a significant amount of time for levels to reach their previous high state. In fact, full recovery can take anywhere from a few months to a year.
Due to low natural testosterone levels after a cycle, most men are advised to undergo a PCT program. This greatly stimulates natural testosterone production and reduces overall recovery time. By itself, this will not bring your levels back to normal; there is no PCT plan on Earth that could do that. However, a solid PCT plan will ensure that you have enough testosterone to keep your body functioning properly while your levels continue to rise naturally. Clomid is an excellent choice for this purpose and one of the most commonly used drugs for PCT. Highly successful PCT programs often include Clomid and Nolvadex, as well as the powerful peptide hormone hCG (human chorionic gonadotropin).
Those who withdraw from Clomid therapy at the end of a cycle or any type of PCT plan and intend to stop the cycle for an extended period of time will rest in low testosterone conditions for an extended period of time. Not only is this a highly unhealthy condition, it can be accompanied by all the traditional symptoms of low testosterone. Many will find that cortisol levels rise significantly as testosterone levels are low, and as a result, body fat levels rise and strength and muscle mass decrease. If you are going to be off a course for an extended period of time, 8 weeks or more, there is no reason to leave the PCT program. If you’re going to quit for less than 8 weeks or switch to a low dose of exogenous testosterone, which is very common in avid bodybuilding circles, this is the only time PCT will be counterproductive.
Side effects of Clomid
Review of clomiphene citrate, clomid is one of the most well tolerated SERMs and antiestrogens on the market and this applies to both men and women. Although it has a very high tolerance threshold, side effects of Clomid exist and are possible. However, “maybe” is the key word and a very important word. Whenever anabolic steroids are discussed, as well as non-steroidal drugs used by anabolic steroid users, many seem to like to assume that side effects are guaranteed. This is not the case; In fact, most of them should be able to use Clomid without side effects.
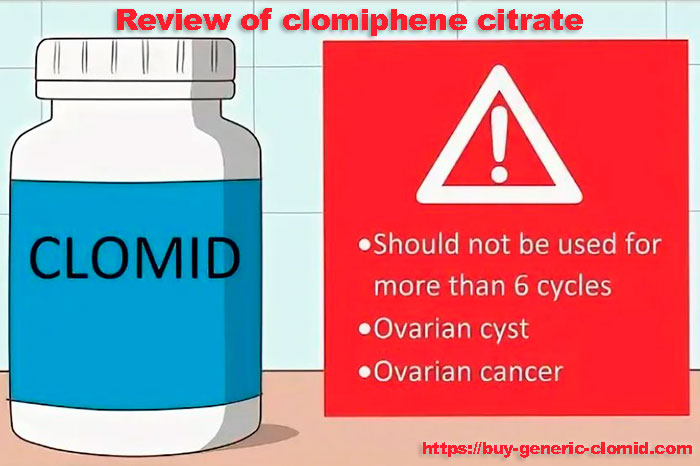
When it comes to the possible side effects of Clomid, we find that most of them are quite rare. Some women who have used SERMs as a fertility aid have experienced ovarian enlargement, but again, this is very rare. Other possible side effects from using Clomid include:
- Headache
- Nausea
- tides
- Uterine bleeding (extremely rare)
- Discomfort in the chest
The side effects of Clomid are also well known in that they include possible visual disturbances. The data show that approximately 1.5% of all those who take Clomid may experience some kind of visual impairment, usually in the form of blurred or blurred vision. In this case, the reception should be stopped and alternative medicines explored. In most cases, vision will return to normal soon after use is stopped. However, in recent years, there have been several cases of visual impairment that did not help to eliminate after discontinuation of the drug. Usually such cases are associated with long-term use of very high doses. Again, if visual disturbances occur, discontinue use immediately and select another SERM that suits your needs.
One last note about Clomid side effects: some may experience acne. This appears to be most common when SERM is used as part of a PCT program. In this case, the problem is not with the SERM, but with the large influx of natural testosterone that is now being produced. Most shouldn’t have a problem, but those who are already genetically sensitive to acne may develop acne on their back, shoulders, or chest.
Review of clomiphene citrate – conclusions: Clomid is an excellent SERM, and for years there has been a debate among anabolic steroid users about which SERM is better, Clomid or Nolvadex. In order to protect against gynecomastia during the cycle, any will do. Some have reported that Nolvadex tends to work better, but you may need to try both at different times to make an accurate assessment. Then we use PCT and both are equally effective and important. Many loudly claim that Nolvadex is a much better SERM for PCT purposes; however, there is a general problem with this statement. Most of those who use Clomid do not use it enough. On a milligram for milligram basis, Nolvadex is stronger, so if you are not planning your Clomid dose to match Nolvadex, you will be disappointed with Clomid. Learn and understand SERMs and various elements before using them.