Nowadays, pregnancy after 40 years is a fairly common phenomenon, however, this is exactly the case when pregnancy should be prepared, and especially carefully.
The ideal age for conception, gestation and birth of a child is entered by specialists in the framework of 22-26 years, it is during this period that the hormonal level is optimal, health is tolerable, there are a lot of eggs and they are healthy. Although at this age, deviations from the norm and problems are possible. Nevertheless, a woman’s reproductive system functions not only during this short period, which means that nature allows her to continue childbirth at an older age, up to the onset of menopause, when the resource of eggs is exhausted and the extinction of all occurs. And taking into account the development of modern reproductive technologies, it is quite possible to give birth to a child after the onset of menopause.
Pregnancy after 40 years risk factors
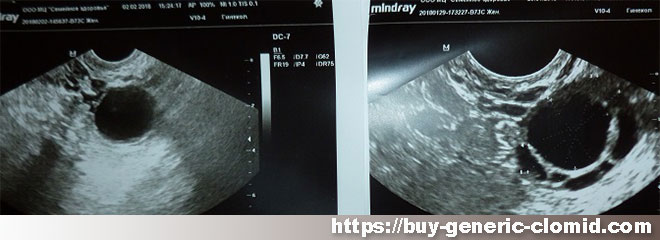
At birth, every girl has a certain supply of germ cells that are consumed throughout her life, which means that the older the woman, the older the follicles stored in the ovaries. Every month, one egg matures and leaves the ovaries, but the remaining follicles are susceptible to aging and external factors, just like any other cells in the body.
This fact is associated with an increased risk of giving birth to a baby with chromosomal abnormalities. Merciless statistics show that the anomaly of the development of the 21st chromosome – Down’s disease in the fetus among women who gave birth at 23-25 is about 1 in 1300, and at 40 it is already 1 in 30. Doctors believe that such statistics also indicate that the mechanism of natural rejection of an embryo with genetic disorders fails with age. And this means that with its full-fledged work, even before the implantation of an egg in the uterus, its removal (chemical pregnancy) would have occurred.
The process of conception itself becomes much more complicated in adulthood, since blood flow to the reproductive organs decreases, the sensitivity of the uterus to sex hormones decreases, some chronic diseases and long-term bad habits, such as smoking, prevent conception and implantation.
It will be especially difficult for women who are planning a pregnancy after 40 years with their first child – gynecologists claim that the reproductive organs, which have been in a state of functional insufficiency for many years, age much faster.
How to prepare for pregnancy
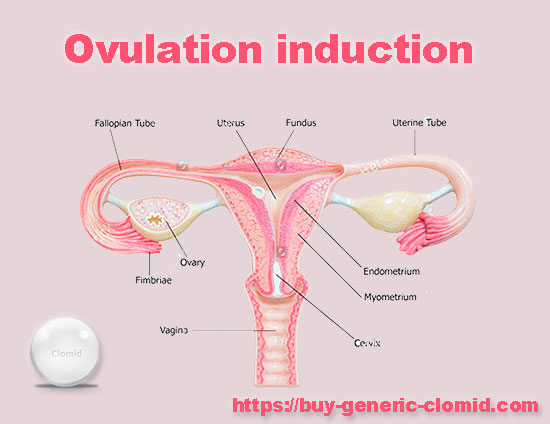
It should be understood that clomid for ovulation stimulation will not solve all problems. First of all, it is necessary to give up bad habits six months before the expected conception, first of all, quit smoking, limit the amount of alcohol and completely abandon all kinds of surrogates, such as low-alcohol and energy drinks.
To give up work that requires strong nervous tension – recent research by scientists suggests that stress at work is one of the factors of problems with conception.

To go in for sports or, at least, to increase physical activity – thus, we increase the elasticity of the joints and strengthen the muscles, which will help to carry and give birth to a baby.
Walk in the fresh air every day, away from car exhaust.
To undergo a full medical examination, in case of chronic diseases, to choose such drugs that are compatible with carrying a child.
To put the oral cavity in order, to cure the teeth. A visit to the dentist during pregnancy is possible, but not at any time and still the risks remain.
Find a doctor you trust, and who will help you prepare for pregnancy and carry a baby.